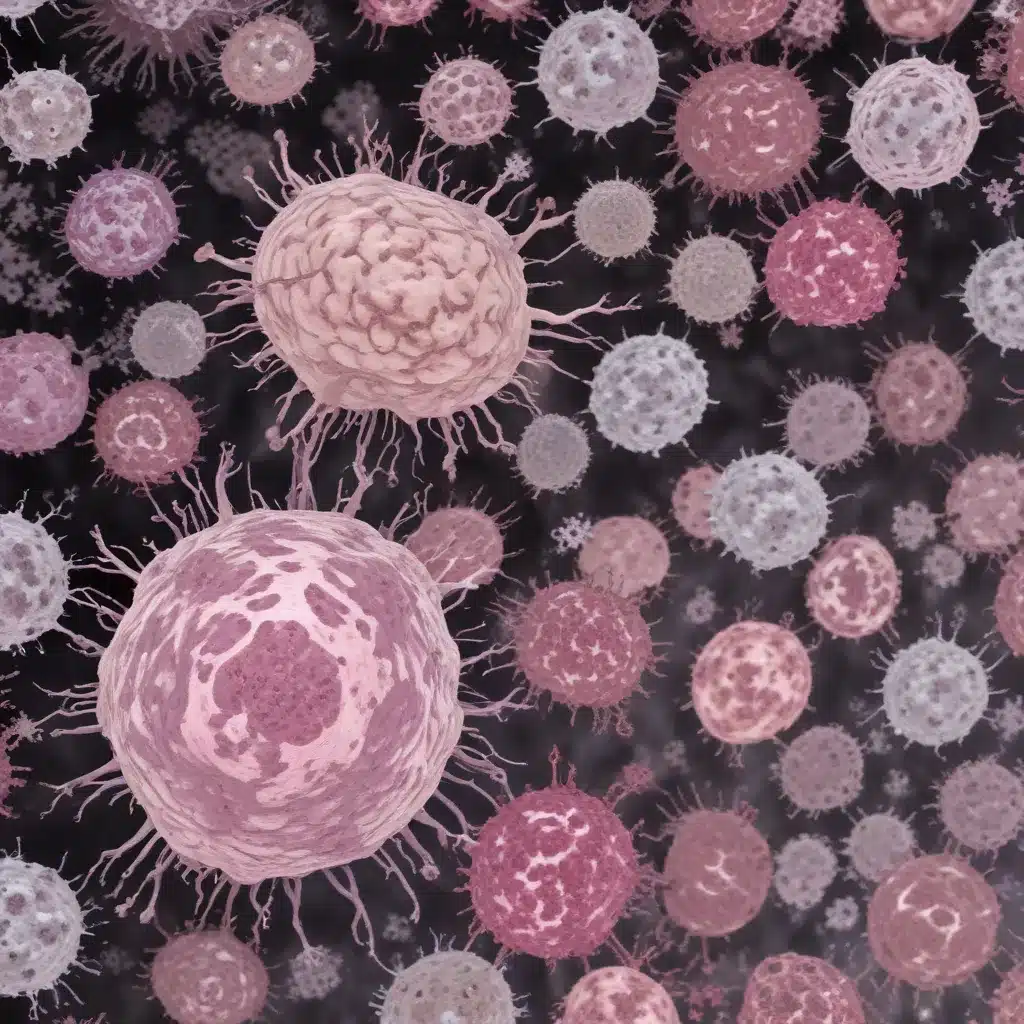
The immune landscape of glioblastoma (GBM) is characterized by a strong immunosuppressive phenotype, presenting a significant challenge for effective immunotherapy. However, recent findings suggest that the expression of the natural killer (NK) cell activating receptor NKG2C, encoded by the KLRC2 gene, could hold the key to enhancing the efficacy of immune checkpoint inhibitors in this notoriously aggressive brain cancer.
Immunological Significance
Activating and inhibitory receptors expressed on the surface of NK and T cells, such as NKG2, NKp, and CLEC, are known to play a critical role in modulating the tumor microenvironment of cold tumors like GBM. Interestingly, a comprehensive analysis of these receptors in GBM samples has revealed a striking overexpression of KLRC2, the gene encoding the activating receptor NKG2C, specifically within the tumor cells themselves. This is in contrast to the significant expression of inhibitory NK receptors observed on the infiltrating immune cells.
The presence of NKG2C on the surface of GBM cells, particularly at the invasive tumor margins, suggests a potential role for this receptor in shaping the immune landscape of the tumor. NKG2C recognition of its ligands could trigger a cascade of events that alters the immunosuppressive microenvironment and facilitates a more effective anti-tumor immune response.
Therapeutic Implications
The discovery of NKG2C expression in GBM cells has important implications for the development of immunotherapeutic strategies. By leveraging the activating properties of this receptor, it may be possible to enhance the efficacy of immune checkpoint inhibitors, which have thus far shown limited success in treating GBM.
Overexpression of KLRC2 in GBM cells was found to be associated with a reduction in the number of immunosuppressive myeloid-derived suppressor cells (MDSCs) and an increase in the presence of tumor-resident lymphocytes. This suggests that NKG2C signaling in the tumor cells themselves can modulate the immune landscape in a way that is more favorable for anti-tumor immunity.
Molecular Mechanisms
The precise molecular mechanisms by which NKG2C expression in GBM cells influences the tumor microenvironment are not yet fully understood. However, existing evidence suggests that this receptor may interact with its ligands to trigger downstream signaling pathways that impact the recruitment and function of various immune cell types.
For example, the activation of NKG2C on the surface of GBM cells could lead to the secretion of chemokines and cytokines that attract and activate cytotoxic T lymphocytes and NK cells. Additionally, the presence of NKG2C may disrupt the immunosuppressive signaling cascades that promote the accumulation of MDSCs and M2-like macrophages within the tumor.
Further research is needed to elucidate the precise signaling cascades and transcriptional programs that are regulated by NKG2C in GBM cells and how these ultimately shape the tumor microenvironment.
Immunotherapeutic Potential
The expression of NKG2C on GBM cells represents a promising avenue for exploiting the immune system to enhance the efficacy of immunotherapeutic approaches. By targeting this activating receptor, it may be possible to unleash a more robust anti-tumor immune response and overcome the inherent immunosuppressive nature of the GBM microenvironment.
Immune Cell Activation
The binding of NKG2C to its cognate ligands on the surface of GBM cells can directly activate NK cells and cytotoxic T lymphocytes, promoting their cytolytic activity and potentially overcoming the effects of checkpoint inhibitory receptors, such as PD-1 and CTLA-4.
Tumor Recognition
The expression of NKG2C on the tumor cells themselves could also enhance the recognition of GBM by the immune system, making the cancer cells more susceptible to attack by immune effector cells. This could be particularly relevant in the context of the infiltrative nature of GBM, where NKG2C-positive tumor cells at the invasive margins may be more vulnerable to immune-mediated destruction.
Cytotoxic Responses
Stimulating the NKG2C-mediated activation of NK cells and cytotoxic T cells could also lead to the release of cytolytic granules and the production of pro-inflammatory cytokines, further amplifying the anti-tumor immune response and potentially synergizing with other immunotherapeutic approaches, such as immune checkpoint inhibitors.
Tumor Microenvironment
The presence of NKG2C on GBM cells appears to have a significant impact on the composition and function of the tumor microenvironment, which is a critical determinant of the response to immunotherapy.
Immunosuppressive Factors
The overexpression of KLRC2 in GBM cells was associated with a reduction in the number of immunosuppressive MDSCs, which are known to hinder the anti-tumor activities of T cells and NK cells. This suggests that NKG2C signaling may disrupt the mechanisms that promote the accumulation of these highly immunosuppressive cells within the GBM microenvironment.
Immune Cell Infiltration
In addition to modulating the myeloid compartment, the expression of NKG2C in GBM cells was also linked to an increased presence of tumor-resident lymphocytes. This enhanced infiltration of cytotoxic T cells and NK cells could improve the overall immune surveillance and responsiveness within the GBM tumor bed.
Tumor Angiogenesis
The interplay between NKG2C signaling and the tumor microenvironment may also extend to the regulation of angiogenesis, as certain NK cell receptors have been implicated in the control of blood vessel formation within solid tumors. The impact of NKG2C expression on the GBM vasculature represents an intriguing area for further investigation.
Translational Applications
The discovery of NKG2C expression in GBM cells has significant translational implications, particularly in the context of developing more effective immunotherapeutic strategies for this devastating disease.
Biomarker Development
The level of NKG2C expression on GBM cells could potentially serve as a predictive biomarker for response to immune checkpoint inhibitor therapy. Patients with high NKG2C levels may be more likely to benefit from these treatments, as suggested by the positive association between NKG2C expression and improved overall survival in the context of PD-1 blockade.
Combination Therapies
Targeting the NKG2C/KLRC2 axis, either through the direct stimulation of this receptor or by leveraging its downstream signaling pathways, could be a promising strategy for enhancing the efficacy of immune checkpoint inhibitors and other immunotherapeutic approaches in GBM. Combination therapies that integrate NKG2C-targeted interventions may help to overcome the inherent resistance of GBM to these emerging treatments.
Clinical Trial Strategies
Future clinical trials exploring immunotherapies for GBM should consider incorporating the assessment of NKG2C expression as a stratification factor for patient enrollment. This could help to identify the subsets of patients most likely to benefit from these treatments and guide the optimization of combination regimens that integrate NKG2C-targeted strategies.
In conclusion, the expression of the NK cell activating receptor NKG2C on GBM cells represents a significant and previously unrecognized aspect of the tumor’s immune landscape. Harnessing the therapeutic potential of this receptor could lead to the development of more effective immunotherapeutic approaches for this devastating disease. As the field of cancer immunology continues to evolve, the NKG2C/KLRC2 axis in GBM deserves close attention and further exploration.



