Endoscopic Retrograde Cholangiopancreatography (ERCP) is a crucial diagnostic and therapeutic procedure used to evaluate and treat various conditions affecting the biliary and pancreatic ducts. As an experienced home improvement consultant writing for Reluctant Renovator, I’ll provide a comprehensive overview of ERCP, including patient selection, procedural techniques, common indications, safety considerations, and quality assurance measures.
ERCP Procedure Overview
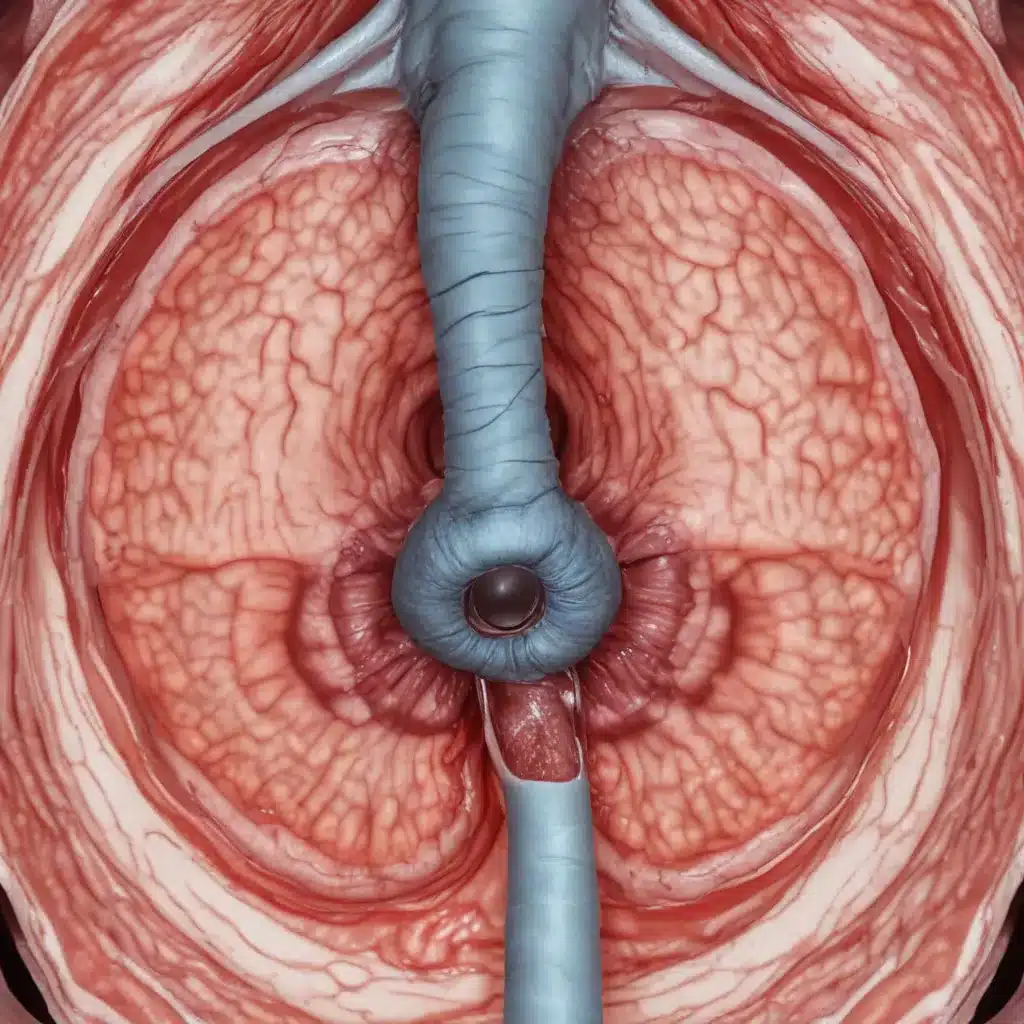
ERCP is a minimally invasive endoscopic procedure that combines the use of a flexible endoscope and fluoroscopic imaging to visualize and access the bile and pancreatic ducts. During the procedure, the endoscopist passes a duodenoscope (a specialized endoscope) through the mouth, esophagus, and stomach into the duodenum (the first part of the small intestine). They then locate and cannulate the papilla of Vater, the opening of the bile and pancreatic ducts, and inject a contrast dye to obtain detailed X-ray images of the ductal systems.
Patient Selection and Preparation
Careful patient selection and thorough pre-procedure preparation are crucial for the success and safety of ERCP. The endoscopist must thoroughly review the patient’s medical history, relevant imaging studies, and laboratory tests to determine the appropriateness of the procedure and identify any potential risk factors. Patients should undergo a comprehensive pre-procedure assessment, including an evaluation of their overall health status, comorbidities, and medication regimen. This helps ensure that the patient is fit to undergo the procedure and that any necessary adjustments to their medication, such as anticoagulants, are made in a timely manner.
Procedural Techniques
The ERCP procedure typically involves several key steps:
-
Sedation or Anesthesia: ERCP can be performed under conscious sedation or, in some cases, with the assistance of anesthesia providers using deep sedation or general anesthesia. The choice of sedation method depends on the complexity of the procedure, the patient’s medical status, and the preferences of the endoscopist and anesthesia team.
-
Duodenoscope Insertion and Cannulation: The endoscopist carefully inserts the duodenoscope through the patient’s mouth, esophagus, and stomach, and then into the duodenum. They then locate and cannulate the papilla of Vater to gain access to the bile and pancreatic ducts.
-
Diagnostic and Therapeutic Interventions: Once access to the ductal systems is obtained, the endoscopist can perform various diagnostic and therapeutic interventions, such as obtaining biopsies, placing stents, removing stones, or performing sphincterotomy (cutting the sphincter muscle to facilitate duct drainage).
-
Fluoroscopic Imaging: Throughout the procedure, the endoscopist utilizes fluoroscopic imaging (real-time X-ray) to guide the interventions and monitor the progress of the procedure.
-
Post-Procedure Care: After the ERCP is completed, the patient is closely monitored in the recovery area for any potential complications, such as pancreatitis, bleeding, or perforation. Patients may be discharged the same day or may require a short hospital stay, depending on the complexity of the procedure and the patient’s medical condition.
Indications for ERCP
ERCP is primarily indicated for the evaluation and management of various biliary and pancreatic disorders. The most common indications include:
Biliary Diseases
- Choledocholithiasis (bile duct stones)
- Biliary strictures (benign or malignant)
- Cholangiocarcinoma (bile duct cancer)
- Bile duct leaks or perforations
- Primary sclerosing cholangitis
Pancreatic Diseases
- Pancreatic ductal stones or calcifications
- Pancreatic duct strictures (benign or malignant)
- Pancreatitis (acute or chronic)
- Pancreatic duct leaks or disruptions
Other Indications
- Evaluation and management of bile or pancreatic duct abnormalities
- Palliative treatment of malignant biliary or pancreatic obstructions
ERCP Safety and Complications
ERCP is considered a high-risk endoscopic procedure, with a reported complication rate of 5-10%. The most common complications include:
Adverse Events
- Post-ERCP pancreatitis: This is the most common complication, occurring in 3-10% of cases.
- Bleeding
- Perforation
- Infection (cholangitis, cholecystitis)
- Cardiopulmonary events (e.g., hypoxia, arrhythmias)
Risk Mitigation Strategies
To minimize the risk of complications, several strategies can be employed, including:
– Careful patient selection and optimization of pre-procedure medical status
– Appropriate use of prophylactic medications (e.g., rectal non-steroidal anti-inflammatory drugs)
– Meticulous procedural technique and adherence to established guidelines
– Prompt recognition and management of adverse events during and after the procedure
Post-ERCP Management
Patients are closely monitored in the recovery area for several hours after the procedure to detect and manage any potential complications. Discharge instructions are provided, and patients are advised to seek immediate medical attention if they develop any concerning symptoms, such as severe abdominal pain, fever, or bleeding.
ERCP Quality Assurance
Ensuring high-quality and safe ERCP services is essential, and this is achieved through a multifaceted approach involving competency-based training, performance monitoring, and continuous quality improvement initiatives.
Competency and Training
ERCP practitioners must undergo rigorous training and demonstrate proficiency in the technical and non-technical skills required to perform this complex procedure. This includes a thorough understanding of pancreaticobiliary anatomy, ERCP indications and contraindications, equipment handling, and management of complications.
Performance Metrics
ERCP providers and units must regularly monitor and report on various performance metrics, such as technical success rates, complication rates, mortality, and patient satisfaction. These metrics are used to benchmark individual and institutional performance against established standards and guidelines.
Continuous Quality Improvement
ERCP providers and units must engage in ongoing quality improvement initiatives, including regular morbidity and mortality reviews, equipment maintenance and reprocessing protocols, and multidisciplinary team meetings to discuss complex cases and identify areas for improvement.
By adhering to these quality assurance measures, ERCP providers can ensure that patients receive the highest standard of care, with a focus on safety, efficacy, and optimal outcomes.
For more information on ERCP and other home improvement topics, be sure to visit Reluctant Renovator.



